Antibiotic resistance is the ability of bacteria to resist the effects of antibiotics. Infections caused by resistant bacteria can be very difficult to treat. When bacteria become resistant to multiple antibiotics that are normally used to treat them, they become "Superbugs".
How Bacteria Become Resistant
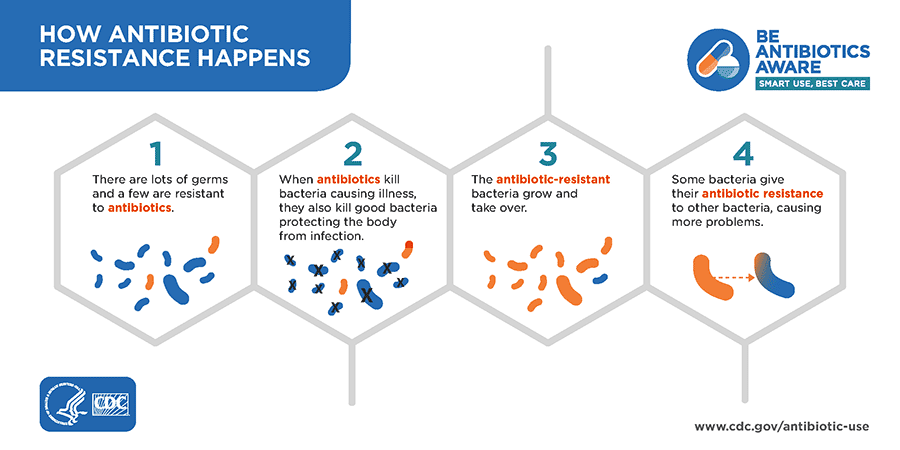
Antibiotic resistance occurs when bacteria change in response to the use of antibiotics, allowing them to survive the effects of antibiotics designed to kill them. If antibiotics lose their effectiveness for these bacteria, then we lose the ability to treat infections and control public health threats.
Antibiotic resistance does not mean the body becomes resistant to antibiotics. Instead, it is the bacteria in the body that have become resistant to the antibiotics designed to kill them.
Why is Antibiotic Resistance Important?
Antibiotic Resistance is one of the most urgent threats to public health. Each year in the United States, more than 2.8 million people are infected with antibiotic-resistant germs, and more than 35,000 people die as a direct result. Many more die from complications from antibiotic-resistant infections.
A growing number of infections – such as pneumonia, tuberculosis, gonorrhea, and salmonellosis – are becoming harder to treat as the antibiotics used to treat them become less effective.
Antibiotic resistance leads to longer hospital stays, higher medical costs and increased mortality. Antibiotic resistance can affect anyone, of any age, in any country.
What You Can Do
- Prevent infections through hand washing, vaccination, and food safety. Wash hands after touching animals or their environment.
- Express your concerns about resistance with your healthcare provider.
Use antibiotics appropriately:
- Do not demand an antibiotic when your health care provider determines one is not appropriate.
- Do not take an antibiotic for a viral infection like a cold, a cough or the flu.
- Take an antibiotic exactly as prescribed. Do not skip doses. Finish taking all of a prescribed antibiotic, even if you are feeling better.
- Do not save any antibiotics for the next time you get sick. Discard any leftover medication once you have completed your prescribed course of treatment.
- Do not take antibiotics prescribed for someone else. The antibiotic may not be appropriate for your illness. Taking the wrong medicine may delay correct treatment and allow a bacterial infection to worsen.
- Always consult your physician about any prescription drug.
What Physicians Can Do
- Talk to your patients about appropriate use of antibiotics.
- Avoid treating viral syndromes with antibiotics, even when patients ask for them.
- Pay attention to dose and duration: the right antibiotic needs to be prescribed at the right dose for the right duration.
- Be aware of antibiotic-resistance patterns in your area so that you can always choose the right antibiotic.
- Include microbiology cultures, when possible, when ordering antibiotics.
- Work with pharmacists to ensure appropriate antibiotic use and prevent resistance and adverse events.
Resources for Healthcare Professionals
- Clinical Recommendations for Common Complaints CDC
- Training and Resources for Healthcare Professionals CDC
- Posters, handouts and patient educational materials CDC

